Understanding Inflammaging: How Inflammation Contributes to Aging
Jan 22, 2026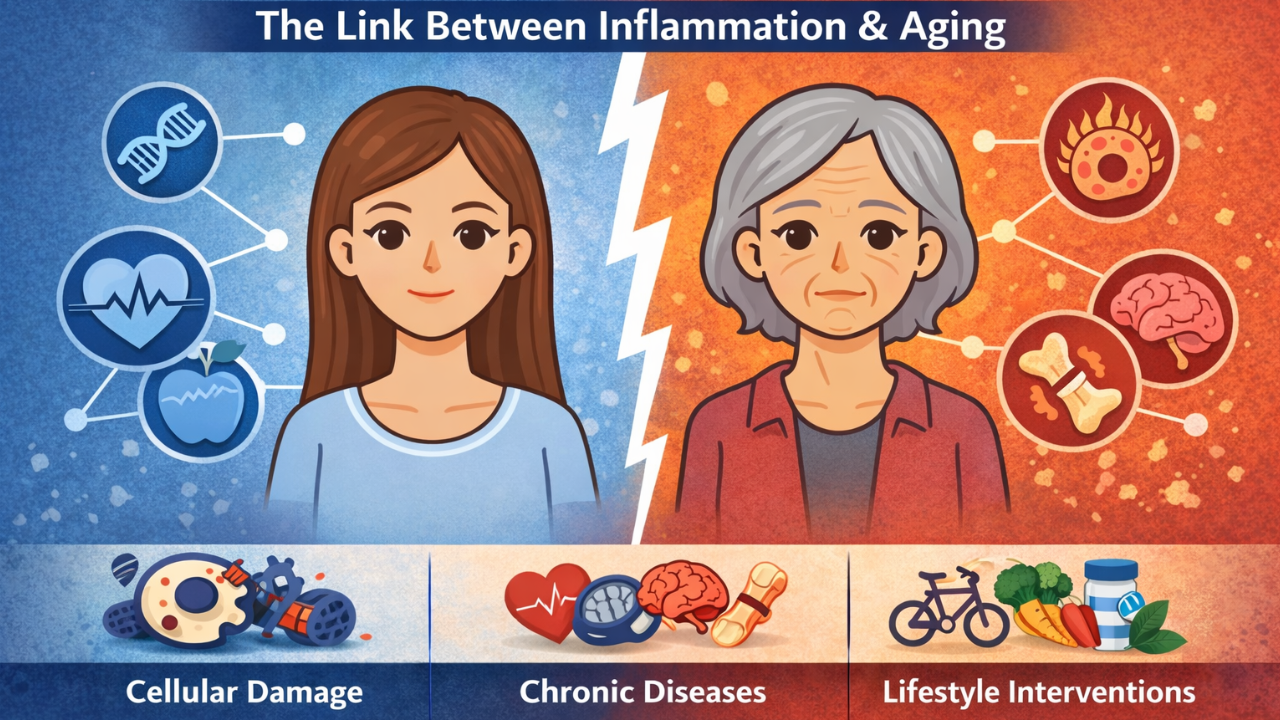
Aging can be understood as a gradual imbalance between damage accumulation and the body’s ability to repair and maintain resilience. Early in life, repair systems are highly effective. Over time, however, ongoing internal and environmental stressors slowly overwhelm these protective mechanisms. One of the most visible consequences of this shift is the persistent activation of the immune system.
This age-related state of chronic, low-grade inflammation is known as inflammaging. Unlike acute inflammation, which is a short-term and protective response to injury or infection, inflammaging occurs in the absence of overt illness. It reflects a long-term immune activation that develops as the body struggles to resolve accumulated cellular and molecular damage.
Importantly, inflammaging is not just a bystander of aging. It is increasingly recognized as both a marker of declining resilience and a driver of age-related disease, contributing to frailty, chronic illness, and reduced health span.
Underlying Mechanisms Driving Inflammaging
Several interconnected biological processes contribute to the development of inflammaging:
Cellular Senescence
As cells experience repeated stress or damage, some enter a senescent state where they no longer divide but remain metabolically active. These cells release inflammatory signaling molecules, collectively known as the senescence-associated secretory phenotype, which can promote inflammation in surrounding tissues and accelerate aging processes.
Mitochondrial Dysfunction
Mitochondria play a central role in energy production and cellular repair. With aging, mitochondrial efficiency declines, leading to increased oxidative stress and release of damage signals that activate immune pathways. Impaired clearance of damaged mitochondria further amplifies inflammatory signaling.
Immune System Dysregulation (Immunosenescence)
Aging alters immune cell populations and function. The immune system becomes less effective at responding to new threats while remaining chronically activated. This imbalance results in persistent inflammatory signaling alongside reduced immune defense.
Gut Microbiome Changes
Age-related shifts in the gut microbiome can increase intestinal permeability and exposure to inflammatory microbial products. Loss of beneficial microbes and expansion of pro-inflammatory species further contribute to systemic inflammation.
Together, these processes create a self-reinforcing cycle in which inflammation accelerates damage, and accumulated damage perpetuates inflammation.
Inflammatory Markers Associated With Aging
Inflammaging is commonly reflected by chronically elevated inflammatory markers in circulation, even among otherwise healthy older adults. These elevations are typically modest compared to acute infection but persist over time.
Markers frequently associated with aging-related inflammation include:
-
C-reactive protein
-
Interleukin-6
-
Tumor necrosis factor–related signaling
Higher levels of these markers have been linked to increased risk of cardiovascular disease, metabolic dysfunction, neurodegenerative conditions, frailty, disability, and mortality. However, research increasingly shows that no single marker fully captures inflammaging, as inflammation varies across tissues and biological contexts.
Newer approaches are exploring patterns of inflammatory signals rather than isolated values, reflecting the complex and dynamic nature of immune aging.
Clinical Considerations: Why Inflammaging Matters
Inflammaging is now recognized as a core contributor to many chronic diseases traditionally associated with aging, including cardiovascular disease, diabetes, neurodegeneration, cancer, and functional decline. From a clinical perspective, inflammation represents both:
-
A signal that resilience mechanisms are failing, and
-
A modifiable biological process that influences long-term health outcomes.
While broad suppression of inflammation can be harmful if it interferes with immune defense, evidence suggests that targeted and lifestyle-based strategies can reduce harmful inflammatory signaling while preserving immune function. Physical activity, dietary patterns such as Mediterranean-style eating, stress regulation, and metabolic health all appear to influence inflammatory burden over time.
Rather than eliminating inflammation entirely, the goal is to restore balance—supporting repair, resilience, and immune regulation. Framed this way, inflammaging becomes a useful lens for understanding biological aging and a practical target for interventions aimed at extending health span rather than simply treating disease.
Director of Education at FMP Essentials
References:
-
Singh A, Schurman SH, Bektas A, et al. Aging and Inflammation. Cold Spring Harb Perspect Med. 2024;14(6):a041197. Published 2024 Jun 3. doi:10.1101/cshperspect.a041197
-
Walker KA, Basisty N, Wilson DM 3rd, Ferrucci L. Connecting aging biology and inflammation in the omics era. J Clin Invest. 2022;132(14):e158448. doi:10.1172/JCI158448


