Menopause, Microbes & Motility: Understanding the Gut–Hormone Link
Nov 07, 2025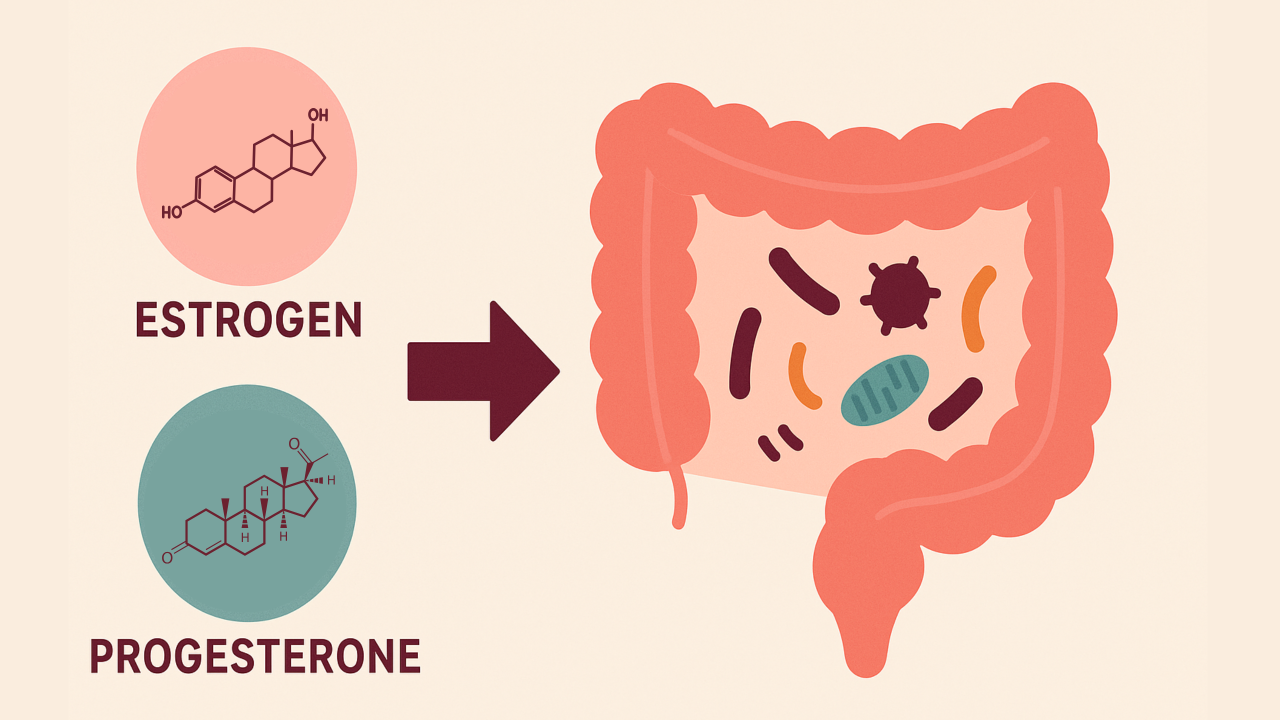
The menopausal transition affects far more than reproductive health. Shifts in estrogen and progesterone during this time influence the gut microbiome, intestinal motility, bile acid metabolism, and barrier integrity in ways that can affect digestion, inflammation, and metabolic health. Understanding this connection helps explain why many women notice changes in digestion and gut symptoms as they approach menopause.
Hormones and the Gut Microbiome
After menopause, women tend to have lower gut microbial diversity and a microbiome composition. These changes are linked to increased inflammation, altered metabolism, and a higher risk of gastrointestinal discomfort such as bloating or constipation.
A key link between hormones and the gut is the estrobolome—the group of gut microbes that produce β-glucuronidase, an enzyme that deconjugates estrogens excreted in bile and allows them to be reabsorbed into circulation. This process, known as enterohepatic recycling, helps regulate how much estrogen remains active in the body.
When estrogen levels fluctuate and decline during perimenopause and menopause, their stabilizing influence on the gut weakens. Low estrogen reduces microbial diversity, alters which bacteria produce β-glucuronidase, and compromises the gut barrier. The estrobolome becomes less balanced and less efficient, disrupting estrogen recycling and creating a feedback loop: low estrogen disrupts the microbiome, and a disrupted microbiome further worsens estrogen balance.
The result is a gut environment that is less resilient, increasing susceptibility to dysbiosis, metabolic changes, and hormone-related symptoms.
Bile Acid Physiology and Hormones
Sex hormones also influence bile acid production and movement, which affects digestion and the microbial environment of the small intestine.
Estrogen supports bile acid synthesis and secretion in the liver. When estrogen levels decline, bile production decreases and its antimicrobial activity weakens, creating conditions that favor microbial imbalance.
Progesterone relaxes smooth muscle, including the gallbladder. In high-progesterone states such as pregnancy, this can slow bile flow and lead to bile stasis. After menopause, when progesterone levels are lower, that inhibition lessens, but bile movement may still remain sluggish because of reduced estrogen and age-related changes in gallbladder tone.
Together, these hormonal changes alter bile flow, microbial balance, and motility—all important factors in maintaining a healthy small-bowel ecosystem.
Estrogen and Gut Barrier Integrity
Estrogen helps maintain the intestinal barrier by supporting tight junction proteins, mucin production, and short-chain fatty acid (SCFA) metabolism. These mechanisms protect the gut lining and regulate immune function. As estrogen levels drop, the gut barrier becomes more permeable, allowing microbial components such as lipopolysaccharides to cross into circulation and trigger inflammation. This low-grade inflammation may contribute to the metabolic and gastrointestinal changes many women experience during the menopausal transition.
Hormone Therapy and the Gut
Emerging research suggests that hormone replacement therapy (HRT) may partially restore microbial diversity and shift the gut microbiome toward a more premenopausal-like profile. Postmenopausal women on HRT (estrogen with or without progesterone) have been shown to have higher microbial diversity and more favorable metabolic markers compared to non-users.
However, these findings remain preliminary. While HRT may help support a healthier gut environment, more research is needed to determine whether it directly improves estrobolome function or gut barrier integrity. Regardless of HRT use, this stage of life is a powerful opportunity to nourish the gut ecosystem—through colorful, fiber-rich foods, daily movement, hydration, stress resilience practices, and restorative sleep. Supporting gut health not only promotes digestion but also enhances overall vitality, hormone balance, and long-term wellbeing.
The Broader Gut–Hormone Connection
Menopause represents a convergence of hormonal, microbial, and motility changes that affect each other in complex ways. Reduced microbial diversity and SCFA production weaken the gut barrier. Slower motility and altered bile flow favor bacterial stasis and overgrowth. Dysbiosis disrupts the estrobolome, further affecting systemic hormone levels.
By recognizing this connection, clinicians can take a more comprehensive approach—one that supports both hormone balance and gut health.
Takeaway
Changes in estrogen and progesterone levels during perimenopause and menopause influence gut health through changes in microbial diversity, bile acid physiology, barrier integrity, and motility. Hormone therapy shows early promise in improving aspects of the gut microbiome, but the evidence remains preliminary. Regardless of HRT use, supporting gut health through balanced nutrition, fiber intake, hydration, regular physical activity, stress management, and adequate sleep remains the foundation for optimizing digestion and overall wellbeing during this life stage.
Director of Education at FMP Essentials
References
-
Peters BA, Lin J, Qi Q, et al. Menopause is associated with an altered gut microbiome and estrobolome, with implications for adverse cardiometabolic risk in the Hispanic Community Health Study/Study of Latinos. mSystems. 2022;7(3):e0027322. doi:10.1128/msystems.00273-22.
-
Zhao H, Chen J, Li X, et al. Compositional and functional features of the female premenopausal and postmenopausal gut microbiota. FEBS Lett. 2019;593(18):2655-2664. doi:10.1002/1873-3468.13527.
-
Lin F, Ma L, Sheng Z. Health disorders in menopausal women: microbiome alterations, associated problems, and possible treatments. Biomed Eng Online. 2025;24(1):84. doi:10.1186/s12938-025-01415-3.
-
Yang M, Wen S, Zhang J, et al. Systematic review and meta-analysis: changes of gut microbiota before and after menopause. Dis Markers. 2022;2022:3767373. doi:10.1155/2022/3767373.
-
d’Afflitto M, Upadhyaya A, Green A, Peiris M. Association between sex hormone levels and gut microbiota composition and diversity: a systematic review. J Clin Gastroenterol. 2022;56(5):384-392. doi:10.1097/MCG.0000000000001676.
-
Chaudhary R, Bansal N, Sharma S, et al. Mechanistic pathways of estrogen mitigating postmenopausal gut dysbiosis. Mol Biol Rep. 2025;53(1):45. doi:10.1007/s11033-025-11179-7.
-
Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: physiological and clinical implications. Maturitas. 2017;103:45-53. doi:10.1016/j.maturitas.2017.06.025.
-
Wang H, Shi F, Zheng L, et al. Gut microbiota has the potential to improve health of menopausal women by regulating estrogen. Front Endocrinol (Lausanne). 2025;16:1562332. doi:10.3389/fendo.2025.1562332.
-
Cross TL, Simpson AMR, Lin CY, et al. Gut microbiome responds to alteration in female sex hormone status and exacerbates metabolic dysfunction. Gut Microbes. 2024;16(1):2295429. doi:10.1080/19490976.2023.2295429.
-
Chaudhary R, Bansal N, Kaur A, et al. Gut microbiota metabolic axis dysfunction in estrogen-deficient stressed rats. Naunyn Schmiedebergs Arch Pharmacol. 2025;398:10.1007/s00210-025-04399-y. doi:10.1007/s00210-025-04399-y.
-
Ley D, Saha S. Menopause and gastrointestinal health and disease. Nat Rev Gastroenterol Hepatol. 2025;10.1038/s41575-025-01075-7. doi:10.1038/s41575-025-01075-7.
-
Becker SL, Manson JE. Menopause, the gut microbiome, and weight gain: correlation or causation? Menopause (New York, N.Y.). 2020;28(3):327-331. doi:10.1097/GME.0000000000001702.
-
Dothard MI, Allard SM, Gilbert JA. The effects of hormone replacement therapy on the microbiomes of postmenopausal women. Climacteric. 2023;26(3):182-192. doi:10.1080/13697137.2023.2173568.
-
Mikkelsen KH, Frost M, Abrahamsen B, Jensen J-EB, Pedersen O, Hansen T. Endocrine aspects of gut microbiota in health and disease. Endocr Rev. 2020;41(3):314-328. doi:10.1210/endrev/bnaa001.
-
Chen J, Yue Y, Wang L, et al. The gut microbiome and menopause: mechanisms and clinical implications. Front Cell Infect Microbiol. 2022;12:879265. doi:10.3389/fcimb.2022.879265.
-
Fuhrman BJ, Feigelson HS, Flores R, et al. Associations of the fecal microbiome with urinary estrogens and estrogen metabolites in postmenopausal women. J Clin Endocrinol Metab. 2014;99(12):E2599-E2607. doi:10.1210/jc.2014-2222.


